
ELSI

About ELSI
ELSI stands for Ethical, Economic, Legal and (Psycho)Social Issues (in Genetics). ELSI research contributes to the strategic ELSI program within the department of Genetics. The ELSI program investigates the (potential) ethical, economic, psychological, social, and legal implications of (new, promising) genetic technologies, as well as methods of diagnostics, counselling (including eHealth), and screening.
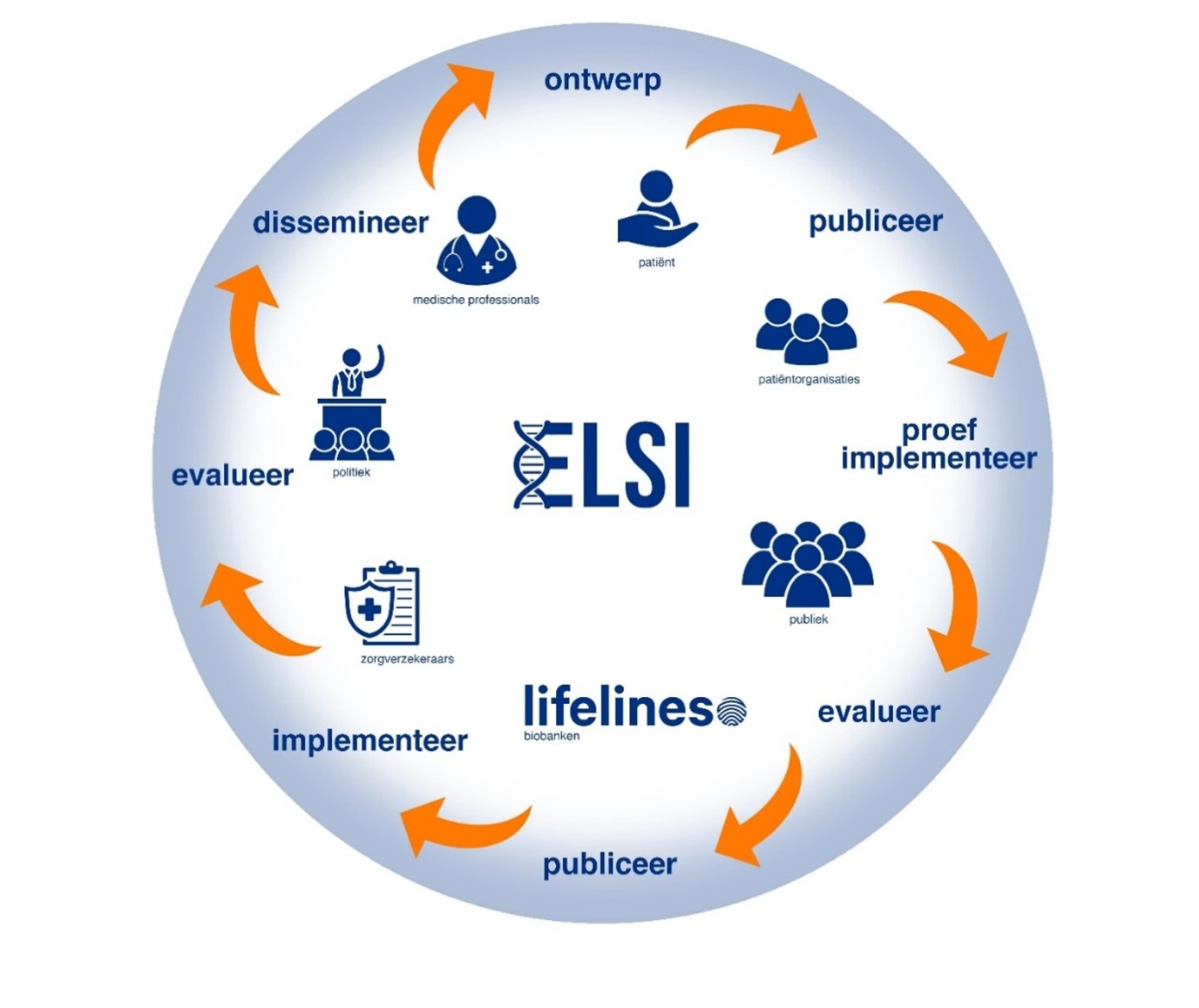
The goal of the ELSI program is to explore, together with all stakeholders, whether and how the aforementioned techniques and technologies can be developed and implemented as quickly and responsibly as possible in order to benefit patients and the public. The program also serves to identify any gaps (e.g. financial or legal) that need to be addressed before responsible implementation can take place. The ELSI research team collaborates on various themes with national and international colleagues. Our research activities not only focus on theoretical and conceptual questions, but also involve pilot studies, trials and finally translation of results to clinical practice (see picture of research cycle). An important aspect of our research is the involvement of all stakeholders, including participation of patients or the general public. More information on these aspects can be found in the description of our research projects. Next to research activities, the strategic ELSI program is dedicated to moral deliberation, patient participation, and education.
Core team
Dr. Imke Christiaans PI/Head of Program (Clinical Genetics, Epidemiology)
Dr. Els Maeckelberghe (Ethics)
Prof. Adelita Ranchor (Psychology)
Dr. Erwin Birnie (Economics, Epidemiology)
Dr. Mirjam Plantinga (Economics, Ethics, Sociology)
Dr. Jacobien Niebuur (Postdoctoral researcher)
Students/Internships
The ELSI research team has opportunities for short-term researchers, interns and trainees. The team is always looking for enthusiastic students who want to perform research on ELSI aspects of genetics. In recent years, students with very different backgrounds (medicine, psychology, philosophy, human technology, science business and policy and communication sciences) have been trainees in the ELSI group. Contact Dr. Imke Christiaans (i.christiaans umcg.nl) for more information.
Research projects
The ELSI in Genetics team’s research concerns various topics. To show the extent of our research, we provide information on some recent and historical research projects below.
1. Screening
Recent project – Responsible employment of next generation sequencing techniques in screening. Next generation sequencing techniques like whole exome sequencing (WES) and whole genome sequencing (WGS) allow the analysis of the entire DNA. WES/WGS-based screening offers opportunities for expanding reproductive choice before and during pregnancy, as well as for promoting early diagnosis of treatable conditions and realizing health gains. It also raises ethical, legal and societal questions. Through a literature review and empirical and normative analysis, carried out in collaboration with relevant stakeholders, this research will identify the conditions for responsible WES/WGS-based screening including the role of the government in realizing these conditions. Three screening settings are central: population screening, opportunistic screening and a commercial offer. For four crucial aspects in these settings (information and consent, quality of screening and secondary findings, re-use of data, and impact of non-participation), we will investigate to what extent further elaboration or adjustment of the existing normative screening framework is needed.
Historical project – Preconception carrier screening in family planning. An example of innovation in Genetics and the different steps of research cycle is the widespread offer of preconception carrier screening to people who plan to have children. On 28 June 2021, Juliette Schuurmans was granted her PhD on this subject. Preconception carrier screening offers couples planning to start a family the possibility to verify, prior to pregnancy, whether they – as a couple – have a significantly increased chance of having children with a serious recessive condition. Such a screening test had not previously been offered or evaluated in a healthcare setting.
This project started with an international multidisciplinary stakeholders’ meeting at which participants turned up the heat on one another about what a responsible test should look like. Subsequently, the lab set up a preconception carrier screening test and the ELSI research group carried out research probing the desirability and conditions for offering such a test under both potential providers and child-planning couples. Apart from some hesitancy, much enthusiasm was expressed. This was followed up by the set-up, execution and evaluation of a pilot in the Northern Netherlands. The pilot showed that responsible implementation is possible in a carrier test offered by general practitioners.
In the next step towards nation-wide implementation, our Dutch consortium developed a Dutch guideline – within a ZonMW study initiated by the Ministry of Health, Welfare and Sports – of advice aimed at conditions for a national trial implementation of preconception carrier screening. This advice has been taken into account by the Dutch Health Council in their report on preconception carrier screening of 15 November 2023, which suggests this screening be offered to all child-planning couples but that the effectiveness and feasibility of such a nationwide offer should first be valuated in a pilot study.
2. Technological innovation
Current project – Pedigree of your heart. The ELSI research group is developing a digital risk-assessment tool that predicts an individual's personal risk of cardiovascular disease based on their family health history. The tool focuses on both monogenic and more complex multifactorial cardiovascular diseases. By implementing this tool, we aim to make people in the general population aware of their personal risk and refer those at higher risk to their general practioner for further diagnostics and treatment so that mortality from sudden cardiac death and severe disease symptoms can be prevented. The tool will be complemented with information for general practioners, and the launch is planned for 2024.
As a first step in tool development, experts mapped the legal and ethical framework and concluded that especially European Union (EU) regulations like the Medical Device Regulation and General Data Protection Regulation present potential obstacles for the tools development, broader availability and general use. The ethical challenge is related to how to warn relatives of a user who might share the same family health history and thus the same risk. Using a focus group and Delphi study, we developed expert-based family criteria that could point towards increased risk and validated them in a high risk and a general population cohort. These family criteria had to understandable for the public and easy to use in a digital tool. Two different tool prototypes have now been developed and tested for acceptance and usability in a general population cohort. This project is funded by the Dutch Heart Foundation.
Current project – ELSA AI Lab Northern Netherlands (ELSA-NN). ELSA-NN is focused on investigating cultural, ethical, legal, socio-political and psychological aspects of the use of AI in the setting of healthcare to promote healthy living, working and ageing. By investigating these aspects in different decision-making contexts via use cases, including one in genetics, and integrating this knowledge into an online ELSA tool, ELSA-NN aims to contribute to knowledge about trustworthy human-centric AI and the development and implementation of health technology innovations, including AI, in the Northern region.
The genetics use case studied within the ELSA AI Lab focuses on the use of AI in variant interpretation in NGS-based newborn screening. Current newborn screening is performed using biochemical tests. With the use of new DNA sequencing techniques, more severe treatable diseases could be screened in newborns. However, with sequencing comes the need to interpret many DNA variants per sample. To allow for a rapid test result, e.g. within a week as in current newborn screening, and given the many samples to be tested, AI can be helpful in interpretation of DNA variants. Which variants can be disease-causing and which are benign? ELSA AI Lab researchers will, together with the ELSI research group, look at legal aspects and ethical and psychological aspects such as trust and acceptance of AI.
More information: ELSA AI lab Northern Netherlands (ELSA-NN) (umcgresearch.org)
3. Counselling
Recent project – Information provision and early detection of relatives at risk of an inherited disease. In many genetic conditions, especially autosomal dominant ones, first-degree relatives have a 50% risk of having the genetic predisposition. Knowing that you have the genetic predisposition can be useful for both life planning and disease prevention. For many hereditary diseases, like hereditary cancer and hereditary cardiovascular diseases, preventive measures and/or treatments are available that can prevent or decrease severe symptoms. However, for such medically actionable hereditary diseases, only 50% of relatives gets tested for the genetic predisposition. The ELSI research group is studying how information provision to relatives can be improved, other reasons they have for not making an appointment for genetic counselling and how we can best help them make an informed decision about genetic testing.
Historical project – Validation of the Genetic Counseling Outcome Scale. Healthcare is now paying more and more attention to measuring patient experiences, for example as recorded by patient reported outcome measures (called PROMs). Several tools are being developed to measure patient experiences in healthcare. However, there was no suitable Dutch tool to measure the effect of genetic counselling on the patient. In the UK, a PROM for genetic counselling had already been developed and validated – Genetic Counselling Outcome Scale (GCOS). The GCOS provides insights into the experiences of patients undergoing genetic counselling. PhD student Jan Voorwinden validated a Dutch version of the GCOS among a large and diverse group of patients, and the ELSI research group has plans to study how the GCOS can be used to further improve counselling experiences, patient empowerment and personalized care.
4. (Re)contacting
Current project – Pharmacogenetic passport. An individual’s genetics can influence how well specific medications work for them. Using genetic information to tailor medication prescriptions can thus help avoid side-effects due to overdosing or lack of effect due to underdosing. In the pharmacogenetics passport project, researchers from the UMCG Genetics department have developed a route to deliver this information to patients or members of the general public via an app. The first pilot will be performed in the participants of the Lifelines biobank for whom DNA is already available. The ELSI research group is evaluating how participants feel about receiving information about their genetic medication sensitivity. We also want to know whether the information in the app is clear and complete so we can better tailor it to people's needs in the future.
Historical project – Duty to recontact. Recontact with patients might be desirable in cases where there are new genetic findings or new interpretations of past findings. A systematic literature study was performed on the duty to recontact and its association with ELSI issues. The review, published in Genetics in Medicine, showed that recontact is desirable, but there is no legal duty to recontact patients. The practicalities of a recontact policy were seen as the most important barrier to its application.
In another study, we conducted interviews with experts and held group discussions with patients and professionals on the duty to recontact and the practical aspects. This study revealed that the participants did not think of recontact as a duty, but that it could be desirable. In addition, we formulated a set of requirements that the recontact policy should take into account for a successful implementation. As a next step a recontacting-app was developed and evaluated in a quantitative study among approximately 250 former patients. The aim was to recontact people efficiently and responsibly when there was new or revised genetic information on their (potential) genetic condition. There are essential medical-ethical, psychological and medical-legal requirements to take into account, including how ex-patients experience recontact and which conditions should be incorporated in eHealth such as a recontacting-app.
| Last modified: | 05 June 2024 12.45 p.m. |
